Oral Presentation The Joint Annual Scientific Meetings of the Endocrine Society of Australia and the Society for Reproductive Biology 2017
Cyproterone vs spironolactone as anti-androgen therapy for transgender females receiving oestradiol therapy. (#62)
Background: Feminising cross-sex hormone therapy improves psychological functioning in male-to-female individuals with gender dysphoria. Oestradiol with or without an antiandrogen (cyproterone acetate or spironolactone) are commonly prescribed in those without orchidectomy. Guidelines for treatment are based on poor quality evidence. We aimed to compare add-on cyproterone versus spironolactone in lowering endogenous testosterone levels in male-to-female transgender individuals.
Methods: A cross-sectional analysis was performed of 114 trans and gender diverse individuals receiving 1) oestradiol alone (n=21), 2) oestradiol plus cyproterone (n=21, or 3) oestradiol plus spironolactone (n=38) for >6 months. We excluded those on GnRH agonists (n=1), previous orchidectomy (n=28), and ethinyloestradiol treatment (n=4) as this was not measurable on our oestradiol immunoassay. Total testosterone level (radioimmunoassay) and secondary outcomes included oestradiol level, oestradiol valerate (Progynova™) dose, blood pressure and renal function. Median (IQR) are reported and differences were tested using Kruskal-Wallis test followed by Nemenyi post-hoc comparisons. A linear mixed model was also fitted with recruiting centre as random effect.
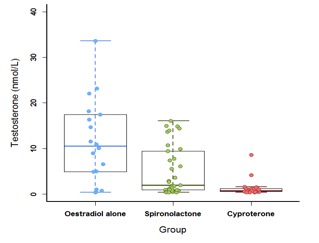
Results: Eighty-one individuals (27.0 years (22.5, 45.1)) were included. Median duration of hormone therapy was 1.5 years (0.9, 2.6). On univariate and multivariable analyses, the cyproterone group had significantly lower total testosterone levels (0.8nmol/L (0.6, 1.20), n=21) compared with spironolactone group (2.0nmol/L (0.9, 9.4), p=0.037, n=38) and oestradiol alone (10.5nmol/L (4.9, 17.2), p<0.001, n=21), Figure 1. No differences were observed in oestradiol level, total daily Progynova™ dose, body mass index, blood pressure, haemoglobin, creatinine, potassium or ALT. Urea was higher in the spironolactone group compared with cyproterone. Median dose of spironolactone was 100mg (87.5, 200), and cyproterone 50mg (25, 50).
Conclusions: Oestradiol plus cyproterone achieved total testosterone levels in the female reference range. As spironolactone may cause feminisation without inhibition of steroidogenesis, it is unclear which anti-androgen is more effective at feminisation. Further prospective studies are required.
Figure 1