Poster Presentation The Joint Annual Scientific Meetings of the Endocrine Society of Australia and the Society for Reproductive Biology 2017
Clinical characteristics of trans and gender diverse individuals attending specialist endocrinology clinics. (#212)
Background: Transgender health is an understudied area with relatively little evidence to guide clinical practice. Understanding the medical and psychosocial characteristics of transgender individuals accessing cross-sex hormone therapy may be useful in tailoring health services to the needs of the trans-community.
We aimed to document the number of individuals seeking cross-sex hormone therapy and understand their demographics and medical comorbidities.
Methods: We performed a retrospective audit of all initial consultations with gender dysphoria presenting to two endocrinologists at a private practice in Melbourne, Australia between June 2011 and December 2016.
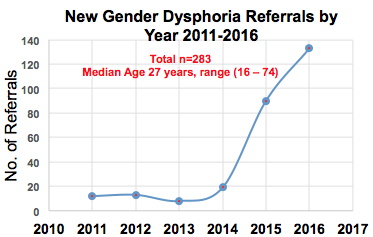
Results: New consultations for gender dysphoria have increased significantly in the last three years (Figure 1) with a total of 283 individuals audited. 17% of patients resided in rural or remote areas across all Australian states. Two-thirds were referred from three LGBTI-friendly GP practices in Melbourne. Median age was 28 years with range (16 – 74). Female-to-male individuals comprised 58% of all referrals, male-to-female 34% and non-binary 8% of trans individuals. Whilst all socio-economic classes were represented, 49% of individuals were either unemployed or students. Medical comorbidities were few with the majority (59%) having a Charlson Comorbidity Index of 0. Conversely psychiatric comorbidities were highly prevalent with 55% being medically diagnosed with depression and 35% diagnosed with anxiety. 24% were currently smoking, higher than the Australian population mean.
Conclusions: There is a rapidly rising demand for endocrinologists to provide cross-sex hormone therapy for trans and gender diverse individuals. Location of patients throughout Australia may reflect a lack of transgender health services. Higher numbers of female-to-male transmen in this specialist endocrinology practice are likely related to current PBS authority guidelines for accessing testosterone therapy. High prevalence of psychiatric comorbidities and relatively social disadvantage support a need for comprehensive multidisciplinary public health services for trans individuals.
Figure 1.