Poster Presentation The Joint Annual Scientific Meetings of the Endocrine Society of Australia and the Society for Reproductive Biology 2017
Sella Dweller (#277)
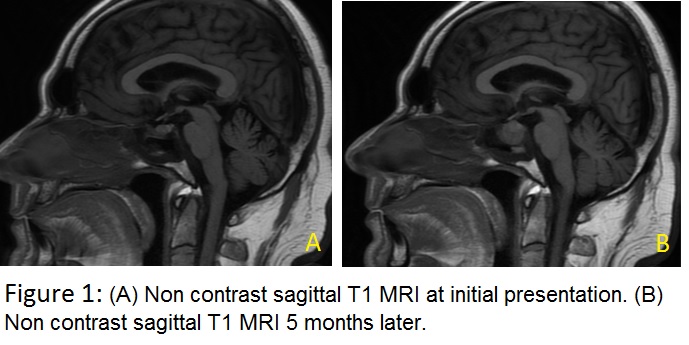
A 56 year-old man presented 4 months post-renal transplant with severe retro-orbital headache. Past medical history included insulin-requiring type 2 diabetes complicated by retinopathy and renal failure. He was immunosuppressed: treatment taken were 4mg tacrolimus, 1000mg mycophenolate and 5mg prednisolone daily. Acceptable glycaemic control was achieved (Hba1c 6.2%; 44mmol/mol.) Non-contrast MRI found normal pituitary anatomy with non-specific sphenoid sinus thickening (Fig1A).
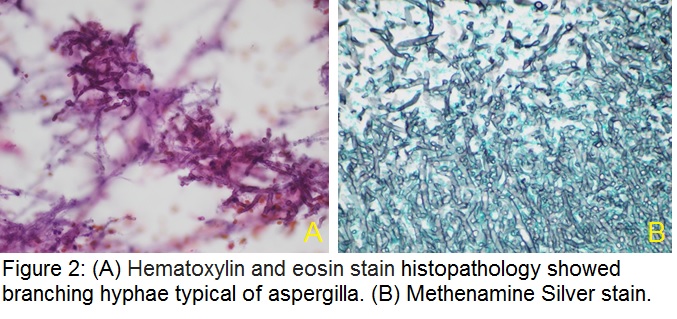
Five months later, following progressive headache, a non-contrast MRI was repeated. This showed rapid enlargement of a hypodense pituitary sella with associated left internal carotid artery narrowing. Sphenoid sinus thickening was more pronounced with a visible fluid level (Fig 1B). Pituitary biochemical profiles showed hypogonadotrophic hypogonadism; other hormones were within normal limits. Two weeks later he presented with an acute cranial nerve III palsy and bitemporal hemianopia. CT brain revealed bony erosion and complete destruction of the sella floor. Trans-sphenoidal pituitary resection was done. Histopathology (H+E stains) showed branching hyphae typical of Aspergillus (Fig 2), confirmed on Methenamine Silver stain (Fig 2B).
Antifungal treatment was given for eight months and immunosuppression was gradually reduced. Repeat MRI demonstrated a significant decrease in the sella mass and sphenoid sinus mucosal thickening but progressive left internal carotid narrowing - suspicious of angio-invasion.
Pituitary fungal infections are extremely rare and often mimic more common causes of sella lesions. Described risk factors are immunosuppression, pituitary surgery and irradiation. Spread can be either haematogenous, contiguous from a sphenoid sinus infection or iatrogenic. Headache is the predominant symptom and aspergillus is the most common offending pathogen. MRI features include a hypo-intense heterogeneous cystic mass on T1 and hyper-intense mass with peripheral ring enhancement on T2. Definitive diagnosis can only be made by histopathology, microscopy and culture but consideration should be given to hormonal replacement and use of antifungal agents if clinical suspicion is high.